Application
A patient-specific, 3D model of pulmonary atresia for surgical planning.
Key Benefits
- Patient-specific model.
- Allows for accurate surgical planning.
- Enables new anastomosis procedure.
Market Summary
Pulmonary atresia (PA), ventricular septal defect (VSD) with major aortopulmonary collateral arteries (MAPCAs) is a rare congenital heart disease associated with heterogeneous and complex forms of pulmonary artery stenosis. Congenital heart defects of any kind affect approximately 1% of all newborns. Current surgical strategy focuses on creating centralized pulmonary artery connections through unifocalization (i.e., anastomosis of the collateral arteries), followed by a right ventricular (RV) to pulmonary artery conduit. Unifocalization surgery can correct pulmonary atresia with major aortopulmonary collateral arteries, but the procedure is difficult and frequently results in pulmonary artery stenosis later in life. However, patient variation is wide and a “one approach fits all” is not possible in this population, thus highlighting the unmet need for patient-specific modeling phantom to enhance surgical planning and develop new surgical methods to treat stenosis.
Technical Summary
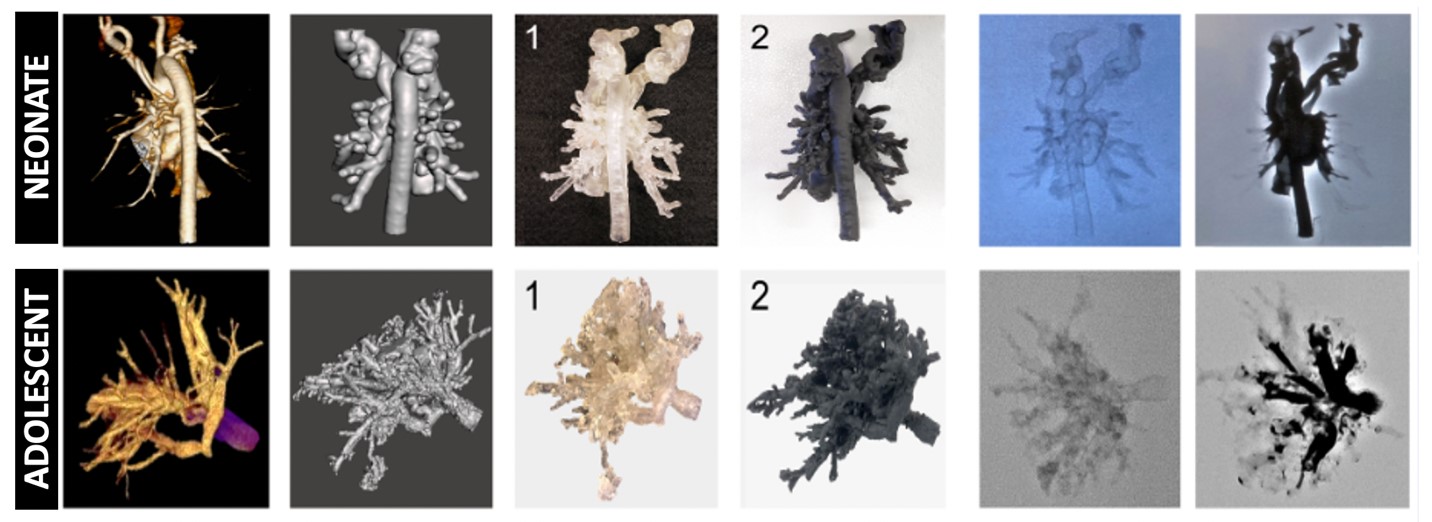
Patient-specific 3D printed models and phantoms of target tissues and organs have shown great potential in improving our understanding of the pathophysiology of the disease and also aid in developing and optimizing surgical treatments. In the case of PA with MAPCAs, in particular, 3D printed models can aid in the visualization of the precise 3D configuration of collaterals and native pulmonary arteries. This is vital for studying the defect and planning corrective surgeries. Emory inventors, using patient imaging data acquired during pre-surgical preparation, constructed 3D digital models of pulmonary vasculature for both neonate (3 days old) and adolescent (14 years old) patients, with resolution that allowed for vascular network and vessel lumen reconstruction, recapitulating those of the in vivo conditions. Multiple synthetic (resin-based) models were reliably printed for neonatal and adult patients with minimal post-processing required, while still maintaining high fidelity patient 3D cardiovascular structures. The protocol to generate these anatomically accurate synthetic phantoms was streamlined to take 2-3 days to complete, making it suitable for use as a clinical aid in planning surgical interventions.
Developmental Stage
3D models have been built and tested in vitro.
Publication: Tomov, M. L. et al. (2019). Journal of the American Heart Association, 8(24).
Read our featured innovation.

